Strengthening a virtual lifeline for Parkinson’s patients
Research explores ways to overcome challenges of online fitness programs
In-person exercise classes can be a lifeline for people with Parkinson's disease, offering vital exercise instruction, an instructor's personal attention and feedback, and a peer group's support and encouragement.
But what happens when that lifeline goes virtual?
That's what Central Michigan University faculty member Jamie Haines is learning in the COVID-19 era — and her discoveries could point the way to better resources for underserved areas of Michigan.
Haines, a board-certified neurologic clinical specialist in physical therapy who teaches in CMU's physical therapy doctoral program, is studying how well people transition to online exercise programs and what factors can help or hurt.
"We wanted to understand and identify perceived barriers and facilitators to exercise during this pandemic, especially in rural Michigan," she said.

An online alternative
Physical exercise is key to slowing the effects of Parkinson's disease. But when COVID shut down community exercise courses in March 2020, most people with Parkinson's disease had nowhere to turn. The Michigan Parkinson's Foundation offered one weekly online exercise class and reached out for help to Haines and a colleague, University of Michigan-Flint physical therapy program faculty member and physical therapist, Dr. Amy Yorke.
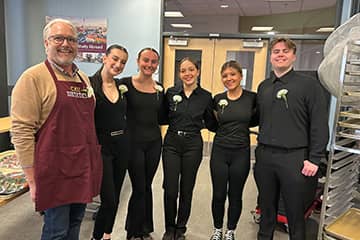
Both had led in-person exercise classes for Parkinson's patients. They quickly shifted gears to help offer online classes six times a week, serving patients across Michigan in Zoom video sessions with up to 50-60 people. At CMU, second-year physical therapy students directing the existing "MOVE! For Health" fitness program for Parkinson's, multiple sclerosis and other neurologic conditions found creative ways to lead exercise from home.
But Haines and Yorke soon realized that not everyone found success online.
"Our research shows that most of our subjects have not returned to or sustained pre-COVID exercise frequencies or intensities even 18 months after the shutdown," Haines said. A therapeutic exercise program aims to raise the heart rate, but patients-in their own at home tended not to work as hard.
"They'd say they'd just turn off their camera and sit down when they felt tired," she said.
Searching for solutions
Haines and Yorke identified people with Parkinson's Disease who were successful in the transition and those who struggled. They set out to follow their progress over 12-18 months through a series of three interviews that started in July of 2020 and recently ended. Five CMU doctoral students conducted the interviews over Zoom.
Their research, submitted for publication, explores factors that made a difference: access to technology, supportive care partners, connections to the Parkinson's community, belief in self, domestic responsibilities such as caring for a spouse, and isolation.
Haines also noted that apathy, loss of motivation, depression and anxiety are common aspects of Parkinson's disease syndrome — all of which may be eased by social interaction and support.
"That was all taken away when we experienced COVID," she said. "Isolation is horrible when you have Parkinson's. It's one of the worst things that can happen for most people with Parkinson's."
Of course, it can be hard for anyone.
"You don't have to have Parkinson's to have all those challenges," Haines said, "and I think our culture is experiencing a lot of that struggle."
She said many of the lessons from their research could apply beyond the Parkinson's community.
New ways to connect
Haines said it comes down to the need to increase connection and accountability online.
"Really, in northern Michigan, the biggest thing is internet access and 'do I have a computer that's updated enough?'" she said. And once the technology is in place, how will people use it to connect?
"The research tells us that checking in with people frequently works, and that's a really big barrier: Who's getting paid to check in on these community members on a more regular basis," Haines said. "Amy and I do it just because it's in our hearts, but it takes time."
The pair also are pursuing grants to buy exercise heart monitors that rural patients could use at home for feedback on the effectiveness of their workout.
Haines said socioeconomic factors definitely have an impact in rural areas.
"We're one of the only classes specific to Parkinson's disease in central Michigan. The resources are much more lacking up here," she said. "This research absolutely fits with CMU's mission to improve health care and services in underserved areas of Michigan."